- Implanted Device Testing
- Loop recorders
- Pacemakers
- Defibrillators (AICD, single and biventricular) and Cardiac Resynchronisation devices
Implanted Device Testing
 These are devices which are implanted for diagnostic or treatment reasons. Usually information about the function of the device is obtained in a clinic. During the clinic visit an interrogating device is placed over it and the information read. Increasingly we can monitor them remotely from the patient’s home and in the future it is likely that clinic visits will be mainly for changes to the programmed function of these devices.
These are devices which are implanted for diagnostic or treatment reasons. Usually information about the function of the device is obtained in a clinic. During the clinic visit an interrogating device is placed over it and the information read. Increasingly we can monitor them remotely from the patient’s home and in the future it is likely that clinic visits will be mainly for changes to the programmed function of these devices.
We have a major practice innovation program in place which is examining how we can incorporate this technology into practice. It promises to improve the quality of care of these patients, particularly those in rural or remote locations.
Loop recorders
These are used to capture infrequent slow or fast heart rhythms causing blackouts or dizzy turns which cannot be detected using Holter ECG monitoring (1-7 days) or surface based (on the skin) Event monitoring (4-8 weeks). These are also used to check that arrhythmias are not recurring after ablation procedures.

Medtronic Reveal
The recorder is implanted just under the surface of the skin of the chest area using local anaesthetic during a simple outpatient procedure. It is small and light and is approximately the size of a memory stick; unlike a pacemaker or AICD, there are no leads inside the heart or blood vessels.

St Jude Confirm
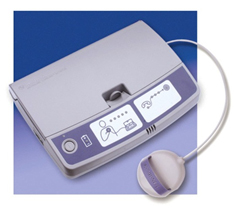
To store an electrocardiogram (ECG) at the time of an episode, a patient places a small hand-held, activator over the device, and presses a button. If the device detects an asymptomatic heart arrhythmia it will also automatically record it. The number of episodes which can be stored varies between devices. The Cardiologist examines the stored information later and determines if the episode was caused by an abnormal heart rhythm. The battery life of these devices is 3 to 4 years and it is removed when a diagnosis is made or excluded.
Remote monitoring uses either wireless technology or a wand to read the device in the patient’s home and sends the data via a land based telephone line to a central monitoring facility and transmits it on to the supervising cardiologist.
Pacemakers
These devices are implanted under the skin of the chest wall and one or two wires travel inside the heart via the veins. They are designed to make the heart beat if the natural pacemaker (sinus node) fails or this electrical activity does not pass from the upper chambers of the heart (atria) to the lower chambers (ventricles) via the heart’s electrical system (AV node and Purkinje system).
Pacemakers have sophisticated inbuilt programs to mimic the normal heart rate responses to emotion, breathing and physical activity and the settings are fine tuned at clinic visits.
An important function of pacemakers is they monitor the function of the pacing leads and the battery in the pacemaker. They also record detailed arrhythmia information which is downloaded from the device at clinic visits unless it is being remotely monitored.
The primary role of the pacemaker is to treat slow heart rhythms. It can also treat fast heart rhythms such as atrial fibrillation (which is a risk factor for heart failure and stroke) but although serious arrhythmias such as ventricular tachycardia or ventricular fibrillation cannot be treated by a pacemaker, the device does record these potentially dangerous events which is a significant help in treating the patient. They require an Automatic Cardioverter-Defibrillator or AICD.
Defibrillators (AICD, single and biventricular) and Cardiac Resynchronisation devices
These devices treat serious and life-threatening arrhythmias and are the most effective way of doing so. They are used either to prevent sudden death in patients at risk of it because of structural heart diseases such as coronary disease or cardiomyopathy (‘Primary Prevention’) or after a near miss clinical event (‘Secondary Prevention’). All AICDs also function as pacemakers if needed ie if the heart slows down excessively.
Defibrillators treat arrhythmias in 2 ways: in the first instance the device tries to stop the abnormal rhythm with a burst of high speed pacing (cardioversion). If that fails, the device will give the heart a shock via the right ventricular lead to reset its rhythm (defibrillation). Patients are usually not aware of cardioversion & nearly always aware of defibrillation.
Since these are life-saving devices we do need to monitor them closely. In particular, we need to ensure that the system (AICD device & leads) is working normally and that inappropriate shocks are minimised.
Some patients with heart failure have a problem with the coordination of the heart’s contraction (dyssynchrony) which makes the left ventricle contract less efficiently. Standard single chamber AICDs only have a lead in the right ventricle which can actually worsen heart failure if the device is needed to pace the heart frequently. Placing a lead in the left ventricle and pacing using both right and left ventricular leads can lead to improvement in the heart’s pumping function. We only use biventricular devices which are also Defibrillators – BiV AICDs.

X-Ray showing the atrial lead (on the upper left) and the left ventricular and right ventricular leads in a patient with a BiV AICD
The devices often record other important information such as atrial arrhythmias (atrial fibrillation) and some devices can detect fluid accumulation in the chest which can be an early indicator of heart failure.
Remote monitoring transmits important information on device function between clinic visits and this supplementary information can be very valuable to the treating cardiologist, family doctor and of course, patient.
